When Your Loved One is in the Intensive Care Unit (ICU)
The Need for ICU: Being in the Intensive Care Unit (ICU) is a very scary and frightening experience. Patients are there because they are critically ill. There are many types of ICU’s, including Medical, Surgical, Neuro(logical), Cardiac/Coronary, Pediatric & Neonatal.
Patients in Medical ICU’s may have conditions such as liver disease, kidney disease, complications from diabetes, gall bladder disease, bleeding ulcers, etc. The Surgical ICU will care for post-operative patients who require critical intensive care. Neuro ICU’s are for patients who have suffered a back/neck injury, stroke, head trauma. Coronary/Cardiac ICU’s would care for patients suffering from some type of heart disease, such as Heart Failure, Heart Attack, coronary surgery. Pediatric ICU’s care for children who require critical care. Neonatal ICU’s care for newborn babies that are born prematurely or sick.
Patient: Nurse Ratio: The ICU patient:nurse ratio is usually 2:1 which means that there is one nurse caring for 2 patients. While this may sound like a small workload for the nurse, it can be quite overwhelming when you are caring for 2 critically ill individuals.
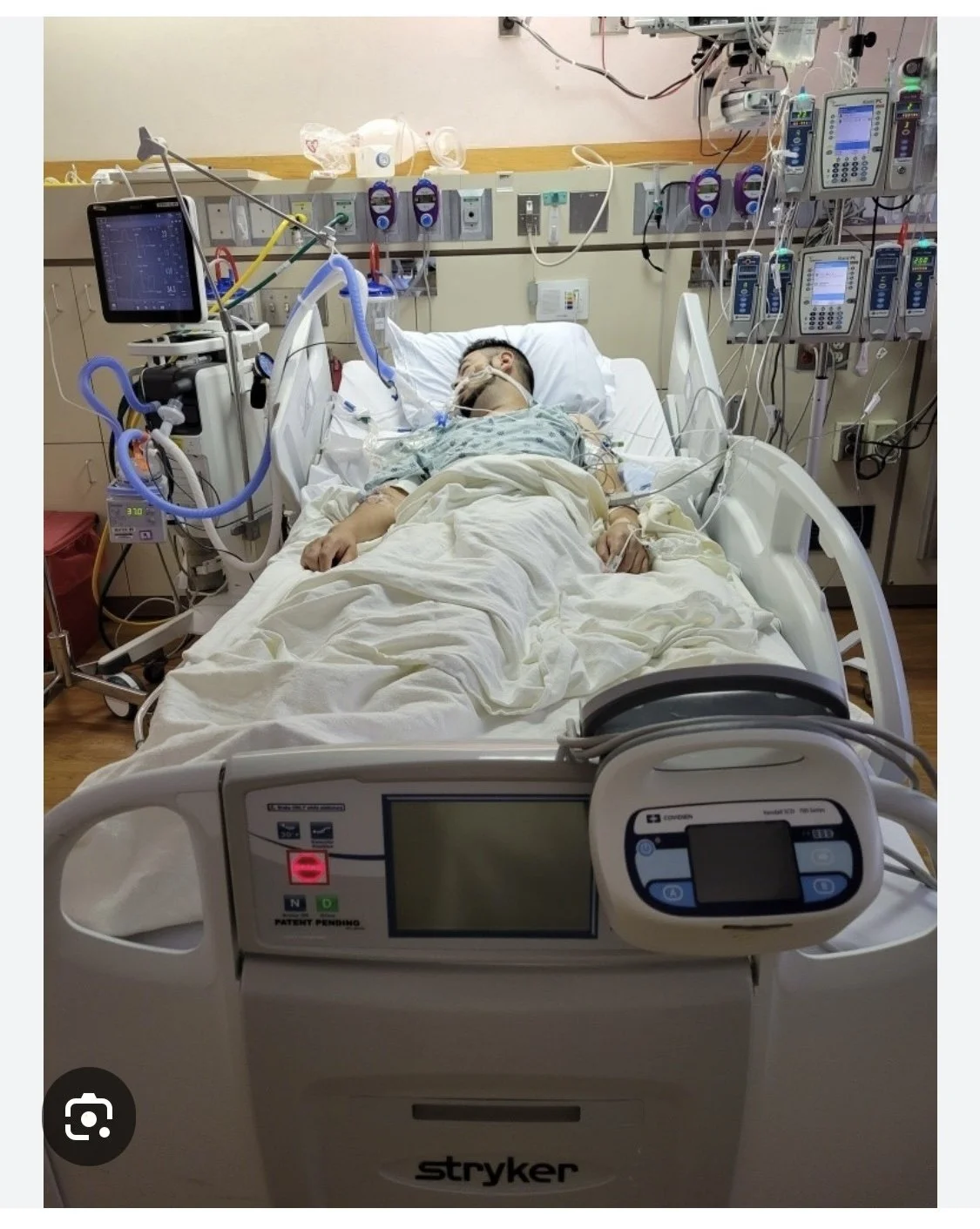
Patient Care Equipment in the ICU: Patients in the ICU are connected to lots of machines & other equipment. One of these machines is a monitor that will measure heart rate (pulse), oxygenation (how much oxygen is in the blood), blood pressure (BP), and breathing rate (respirations). These monitors will often “ring” or “beep”, seeming like quite a nuisance, but they help the staff keep track of important patient information. The staff is able to view these monitors from various places within the ICU.
The patient will also have one or several Intravenous (IV) Lines inserted into an arm or their neck for the administration of fluids, medications or blood. They may have more than one bag of IV solution hanging at more than one time.
The patient may be receiving oxygen therapy. This can be administered through a facial mask or nasal cannula ( small tube).
Patients may have a tube down their nose (nasogastric tube) or inserted directly into the stomach ( gastrostomy tube) which can be used for feeding purposes or for suctioning of stomach contents. This tube may or may not be hooked up to suction.
Patients may have an indwelling foley catheter inserted through their urethra and into their bladder for the purpose of promoting urinary drainage. The tube will be hooked up to a urinary drainage bag hanging off the side of the bed. NEVER raise the bag of urine above the level of the bladder as the back flow of old urine back into the bladder can cause a bladder infection.
Patients may sometimes have a chest tube inserted through the wall of their chest. The purpose of such a tube is usually to reverse a “collapsed” lung. Just for the record, lungs themselves don’t really collapse. What collapse are alveoli which are small air-filled sacs. The tube will be attached to a water filled gravity/suction drainage container. DO NOT DISCONNECT THE TUBE; DO NOT KNOCK OVER THE CONTAINER. This may cause the lung to re-collapse.
Some patients may have a tube down their throat (endotracheal tube) or a tube in a hole made in their neck ( tracheotomy) which may be hooked up to a machine called a ventilator that helps them breath or actually breaths for the patient. Visitors should be aware that the patient will be unable to speak with such a tube in their throat or neck.
Most nurses in ICU’s work 12 hour shifts. Shift changes usually occur between 6:00am/pm and 8:00 am/pm, which means that the nurses and doctors are not available at those times as they are giving report on their patients and/or making rounds. At these times, the staff need to share information with each other that is critical for the safety and continuity of care of patients. Be assured that your nurse will check with you before the shift change to address any needs or questions that you or your family may have before he/she leaves at the end of their shift. and of course, if there's an emergency, they will make themselves available.
QUIET TIME: Some ICU’s have Quiet Time during the change of shift at which time hall lights are dimmed and visitors and patients are asked to refrain from disturbing the staff unless it is something important to the well being of the patient. The Quiet Time is also to give patients a break from the stress and fatigue of daily care routines. Patients are encourage to rest during this Time and visitors are encouraged to take a break from the unit.
Infection Control in the ICU: Thousand of patients die each year from hospital-acquired infections. That means they didn’t come into the health care setting with the infection — they acquired it while they were in the health care setting. Hand washing remains the number one way to reduce the risk of getting or spreading such infections. You should wash or sanitize your hands EVERY time you enter or leave the patient’s room. There may be times when you need to wear a gown and gloves before you enter a patient’s room. This is called “Contact Precautions”. If the patient has a respiratory infection, you may even be asked to wear a mask. The staff will provide you with instructions on what protective items you may need to wear. Be mindful that if you are gowned and gloved, you should not leave the room with the gown and gloves on.
ROUNDS: Throughout the day, multiple health care team members will visit and care for the ICU patients. These team members include physicians, nurses, physical therapists, respiratory therapists, just to name a few. Please remember to ask questions and express any concerns you have when your own health care team visits your bedside. Bring paper and pen with you so you can write down your questions and be sure to get them answered. If you miss those rounds, ask the bedside nurse to have the appropriate doctor call you to give you an update. The doctor that cares for your loved one is called a hospitalist or intensivist.
VISITING IN THE ICU: Each ICU has their own visiting procedures. Become familiar with those in your ICU. They should be posted in the waiting area. Speak to the nurses. While visitors are welcome, there are times when you might be asked to leave. Especially during discussions of confidential nature unless you have been designated as the Patient’s Advocate or Health Care Proxy… of if the patient consents to have you stay. Visitors are often limited to 2 at a time in ICU’s. This is to prevent the patient from getting too exhausted, overstimulated or stressed out. Many hospitals have specially trained staff that will assist with children for what to expect while visiting the ICU. Many ICU’s will not allow anyone under 18 into the unit for fear of exposure to infection. Remember that you need to be sensitive to the patient’s condition while visiting. Patients who are critically ill or recovering from such illness, require lots of rest.
SPENDING THE NIGHT WITH YOUR LOVED ONE: Ask the ICU staff about the policy for spending the night with your loved one. If you don’t get a satisfactory response from them, ask to speak with the ICU Nurse Manager. Oftentimes, there will be a bed or recliner in the room that will accommodate a single visitor. If you do spend the night, don’t be afraid to ask for a pillow and blanket.
PATIENT ADVOCATE OR SPOKESPERSON: While each member of the family has a vested interest in their loved one, it is not fair to expect the staff to answer the same questions or share the same information over and over again with multiple family members. Your family should select one person to act as your family spokesperson. This individual will partner with the staff as part of the patient’s health care team and will disseminate information accordingly to the rest of the family. If the patient has no family or friend advocate with them, an independent patient advocate would be a great resource. Find such an advocate in your geographical area by visiting www.GNANOW.org
PERSONALIZING THE PATIENT’S ROOM: It is not uncommon for your ICU space to become cluttered with patient care equipment. As such, there is little room for personal items. Ask your nurse about personalizing your loved one’s room. If the room is cluttered and small, additional clutter can get in the way of patient care. If space does allow for it, feel free to bring in photos, cards, artwork can be taped to the wall with painter’s tape. A source of favorite music can be very relaxing and soothing. Valuables are encouraged to be left home as their security cannot be guaranteed. Lives plants are usually not allowed in the ICU. Balloons get in the way.